 A year ago, an article in the Calgary Herald reported a 20 percent increase in non-urgent MRI wait times from 2015-2016. The cost to the healthcare system was $59.7 million dollars a year and the average wait times increased from 24 to 35 weeks. Ninety percent of patients had to wait close to 9 months for a non-urgent MRI. This represented a 13.5% year over year increase and which prompted Alberta Health Care Services officials to review physician practices to determine the reason for the increase. Many of these tests were ordered to investigate low back pain. Interestingly, one study conducted in 2013 by Alberta researchers showed that more than 50% of MRIs done for low back pain were either unnecessary or of questionable value.
A year ago, an article in the Calgary Herald reported a 20 percent increase in non-urgent MRI wait times from 2015-2016. The cost to the healthcare system was $59.7 million dollars a year and the average wait times increased from 24 to 35 weeks. Ninety percent of patients had to wait close to 9 months for a non-urgent MRI. This represented a 13.5% year over year increase and which prompted Alberta Health Care Services officials to review physician practices to determine the reason for the increase. Many of these tests were ordered to investigate low back pain. Interestingly, one study conducted in 2013 by Alberta researchers showed that more than 50% of MRIs done for low back pain were either unnecessary or of questionable value.
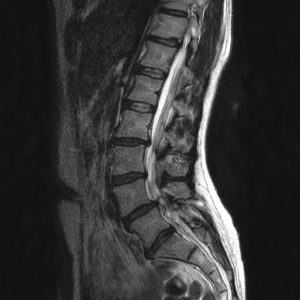
Often times, patients, especially with persistent pain will ask if an MRI should be ordered either prior to starting physiotherapy treatments or as a necessary adjunct to continuing treatment. The reasoning is that the results from an MRI is necessary to determine or affirm a diagnosis and from which a treatment plan can then be more accurately created. At first, this seems reasonable and logical. However, in most instances of musculoskeletal practise, advanced radiology like MRIs are either unnecessary or at worst, create incorrect and confusing diagnoses that have nothing to do with the patient’s actual problem. In other words, so-called “positive” findings like “degeneration” or “partial tears” or “tendinopathy” or “disc bulges” may be inconsequential to the patient’s actual problem and create unwarranted fear and anxiety in the patient. Furthermore, the lack of positive findings rarely provide re-assurance to patients; instead, they only frustrate patients further.
The Canadian Association of Radiologists (CAR) have developed referral guidelines to assist clinicians in making appropriate referrals for imaging studies. The presence of pain only but without other necessary criteria would not be considered an appropriate referral. What would these criteria be? For the lumbar spine, these are:
1. Declining neurological function: The patient demonstrates a worsening of nerve symptoms such as numbness, tingling and weakness.
2. Spinal cord compression: The patient may be losing control of his bowel and bladder function or is demonstrating signs and symptoms of severe or progressive spinal cord deficits.
3. Suspected spinal infection.
4. Suspected cancer.
As you can see from this list, the presence of pain only or even the presence of a single nerve root sign or symptom that is not severe, progressive and declining, do not require advance radiology. Fortunately, clinicians have been well trained to screen patients for those conditions that do require immediate referrals for radiology. For non-emergent conditions then, is it possible to treat conditions like low back or shoulder pain without advanced radiology? Absolutely. This is why physiotherapists spend a large portion of the initial assessment asking questions and completing a thorough physical examination in order to determine the best course of action for each patient. An astute physiotherapist will always ask themselves the following questions:
1. Is this condition emergent?
2. Does the condition require a consult by a family or emergency physician?
3. Does the condition meet the criteria for diagnostic imaging?
4. Would the results of advanced imaging alter one’s clinical decision making and course of action?
If the answer is no to all of the above questions, and if the condition is appropriate for physiotherapy care, then arriving at a diagnosis in musculoskeletal practise involves the creation of clinical impressions from information gathered both from the patient history and the physical examination. In the majority of cases, in these non-emergent conditions, the addition of imaging would not contribute anything different or positive to the patient’s overall care.
Incidentally, it has been shown repeatedly in research studies that many findings on imaging exams such as “degeneration”, “narrowing”, “disc bulge” may have little or nothing to do with the patient’s actual problem. In fact, many of these findings are common in people with no symptoms whatsoever. They may be merely incidental like wrinkles on one’s forehead. Any and all imaging findings must be correlated to the physical examination and history of the patient’s complaints.
Here at Elevation Physiotherapy, both Albert and Karen Chan have a combined 38 years of experience and which includes a combined 17 years of working alongside physicians and specialists in multidisciplinary settings. These advanced practise settings specialize in injection procedures involving ultrasound guidance. Radiology is often used in these settings and so, our determination of clinical impressions and diagnoses and treatment plans have been informed by and strengthened through this process. As well, both of us have been authorized by Physiotherapy Alberta to order diagnostic imaging which includes X-rays, MRIs and ultrasound imaging. Our ability to refer for diagnostic imaging is a great privilege but also a great responsibility. We endeavour to take special care to refer our patients only according to the CAR guidelines.
Submitted by Albert and Karen Chan
